New at Noyce Consulting
The Right Move: Maintenance Home Health
Don't miss this opportunity to see how you can better serve patients and avoid the frequent-flyer syndrome some patients experience when they are discharged from home health only to decline and...
The Right Move: Maintenance Home Health
Don't miss this opportunity to see how you can better serve patients and avoid the frequent-flyer syndrome some patients experience when they are discharged from home health only to decline and...

Don't withhold home health entitlements from qu...
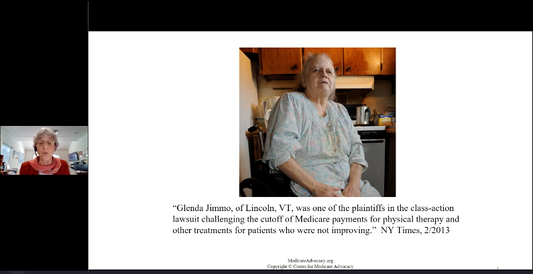
The Center for Medicare Advocacy (CMA) continues working to increase access to home health and hospice services for qualified beneficiaries who, unfortunately, are denied access to their Medicare entitlements based...
Don't withhold home health entitlements from qu...
The Center for Medicare Advocacy (CMA) continues working to increase access to home health and hospice services for qualified beneficiaries who, unfortunately, are denied access to their Medicare entitlements based...

Don't forget to comment on OASIS-C2!
OASIS-C2 replaces OASIS-C1/ICD-10 January 2017, in whatever final form it takes. You can help determine what that final form will be if you submit your OASIS-C2 opinion and ideas to...
Don't forget to comment on OASIS-C2!
OASIS-C2 replaces OASIS-C1/ICD-10 January 2017, in whatever final form it takes. You can help determine what that final form will be if you submit your OASIS-C2 opinion and ideas to...

Palmetto: HbA1c Twice Yearly For DMII Patients ...
For services on or after may 5, 2016, Palmetto will require only two HbA1c tests annually for patients with diabetes mellitus type 2 (DMII) who have "two [quarterly] consecutive HbA1c...
Palmetto: HbA1c Twice Yearly For DMII Patients ...
For services on or after may 5, 2016, Palmetto will require only two HbA1c tests annually for patients with diabetes mellitus type 2 (DMII) who have "two [quarterly] consecutive HbA1c...
