New at Noyce Consulting
PRESSURE INJURY -- It's the New Pressure Ulcer
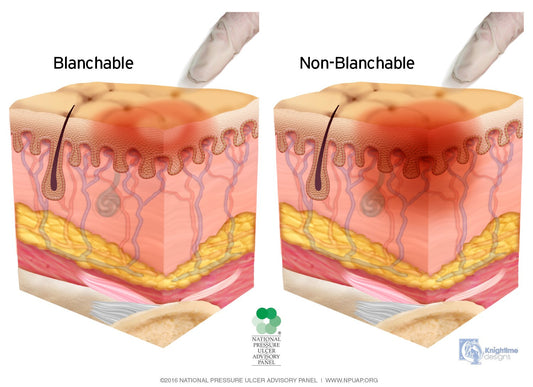
Say "good-bye" to pressure ulcers. Say "hello" to pressure injuries -- in Technicolor! The infamous, only-wounds-to-stage skin lesions are now called "pressure injuries" an April 13, 2016 National Pressure Ulcer...
PRESSURE INJURY -- It's the New Pressure Ulcer
Say "good-bye" to pressure ulcers. Say "hello" to pressure injuries -- in Technicolor! The infamous, only-wounds-to-stage skin lesions are now called "pressure injuries" an April 13, 2016 National Pressure Ulcer...

Deductibles, 20 Percent Copays for Hospice and ...
"Oops, Congress changed that. Hospice isn't covered at 100% any more. Your husband's nurse will collect your 20% hospice co-payment, each visit, Mrs. Jones. And the Social Worker will bring...
Deductibles, 20 Percent Copays for Hospice and ...
"Oops, Congress changed that. Hospice isn't covered at 100% any more. Your husband's nurse will collect your 20% hospice co-payment, each visit, Mrs. Jones. And the Social Worker will bring...

Home Health Can Save Medicare If We Demand a Se...
Medicare's "Independence At Home" demonstration is studying whether providing chronically ill patients with in-home visits by primary-care providers results in both enhanced care delivery and cost savings. I applaud this...
Home Health Can Save Medicare If We Demand a Se...
Medicare's "Independence At Home" demonstration is studying whether providing chronically ill patients with in-home visits by primary-care providers results in both enhanced care delivery and cost savings. I applaud this...

No Fooling! Register for HHCAHPS by April 1 or ...
Home Health Compare 5-Star Ratings grade patient satisfaction survey data in addition to the quality of care that agencies provide to patients. Agencies who aren't registered in the program by...
No Fooling! Register for HHCAHPS by April 1 or ...
Home Health Compare 5-Star Ratings grade patient satisfaction survey data in addition to the quality of care that agencies provide to patients. Agencies who aren't registered in the program by...

Recertify Agency Enterprise Identity Management...
If security officers in every hospice and home health agency don't act by March 15, their agencies will be unable to comply with requirements to file cost reports (home health)...
Recertify Agency Enterprise Identity Management...
If security officers in every hospice and home health agency don't act by March 15, their agencies will be unable to comply with requirements to file cost reports (home health)...

The Whats, Whens, & Hows of Repaying Agency-Dis...
During a spot-check quality audit, you discover that the documentation in the patient record doesn't support the amount Medicare paid for the claim. Alarmed, you search the record for any...
The Whats, Whens, & Hows of Repaying Agency-Dis...
During a spot-check quality audit, you discover that the documentation in the patient record doesn't support the amount Medicare paid for the claim. Alarmed, you search the record for any...
