The Hospice Outcome Patient Evaluation is a step closer to implementation.
After four years of considering options, the Technical Expert Panel (TEP) has finished its work that will inform future Hospice Quality Reporting Program results. The TEP considered quality measures to include in hospice’s future assessment tool and best choices for risk adjustment and exclusion.
The panel convened in 2019 “[we are] committed to improving the quality of care given to hospice patients,” says the 2022-2023 TEP Summary Report: Hospice Quality Reporting Program. The panel aimed to ensure that hospice quality measures are meaningful for hospice beneficiaries, transparent to hospice providers, and useful to consumers. They considered quality measures from both HOPE and claims data.
“From day one it was very clear Medicare wanted to make this a very different experience for hospice teams and make it a more valuable thing for consumers,” says Dr. Jeff McNally, Hospice Medical Director at Utah’s Intermountain Hospice,” describing his participation on the HQRP TEP. “I was actually encouraged and inspired by it,” he says. “It was the first time I had first-hand experience working with any kind of CMS entity.
“The reality is some clinicians in the field and leaders don’t have the best things to say about CMS,” he explains, but “whatever we were considering we always circled back to whether it would be burdensome to the clinical team and would it be valuable to consumers.”
The panel initially planned to meet multiple times in person, with two meetings per year and potential virtual meetings as needed. “Then COVID hit,” Dr. McNally says. “It slowed the process considerably. We never did meet again in person.”
The HQRP TEP met eight times over four years, virtually after the initial meeting. McNally described participants as coming to each meeting prepared with data and proposals for HOPE measures for which they would request input from panelists.”
From TEP recommendations early in their work, Abt Associates developed two outcome measures and two process measures in harmony with hospice’s central tenet to manage symptoms:
- Process measures:
- Timely Reassessment of Pain Impact
- Timely Reassessment of Non-Pain Symptom Impact
- Outcome measures:
- Timely Reduction of Pain Symptom Impact
- Timely Reduction of Non-Pain Symptom Impact
“The most important [recommendations] were some of the outcome measures about symptom management,” McNally explains. “What should we be helping agencies show that they’re doing well? And how do we do that? Deciding which ones, and how many symptom management measures to use and the most valuable way to show it in a fair way.”
During the past two years, TEP members prioritized which of the risk-adjustment factors suggested by Abt. Associates should apply to outcome measures and which exclusions should apply to both outcome and process measures.
The report describes risk adjustment as using statistics to exclude “confounding factors,” or elements that are outside of a hospice’s control, from calculations that could make a hospice’s performance appear either better or worse than it is. In essence, risk adjustment increases the fairness in outcome-measure calculations while exclusions do the same for both outcome and process measures.
For the outcome measures being considered, the report says that the “TEP broadly agreed that risk adjustment is very important because it accounts for external factors outside hospices’ control and more accurately reflects the quality of care provided.”
Judi Lund Person, Principal of LundPerson & Associates, LLC, agrees. “The discussion of risk-adjustment factors is vitally important to the success of upcoming process measure implementation,” says Lund Person.
Determining which risk-adjustment factors to bring to the table was not easy. “There were some nuance things that we hashed out to try and decide how to weigh some factors in risk adjustment” for outcome measures, McNally explains.
Exhibit 5 (below) summarizes the TEP’s rankings of risk adjustors suggested.
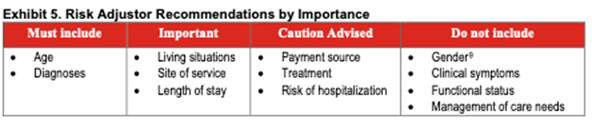
While the TEP’s priorities seem clear, the discussion concerning each risk adjustor was more complex. The TEP broadly agreed that the most important risk-adjustment factors are age and diagnosis. Some diseases are more difficult to manage than others, and patient condition tends to decline with age regardless of provider activity. Therefore, the TEP recommended that CMS adjust for these factors to ensure that common external factors do not adversely affect reported hospice care quality.
Here’s part of the nuance – the TEP also raised concerns that how well other patients with certain diseases or of certain age groups are treated might be valuable to some patients and their families seeking care for someone of the same age group or condition. Panelists fretted over possibly obscuring that information for consumers seeking hospice care by adjusting for those risk factors.
Living situation as a risk adjustor ranked as important to TEP members because hospices have no control over what level of assistance is available to patients. Similarly, site of service ranked high as a risk adjustor because, said some panelists, care is delivered very differently across settings, and patients and/or caregivers tend to provide higher hospice satisfaction ratings for hospices in home settings than for those in facilities,” according to the report.
Lund Person, who is also former Vice President of Regulatory and Compliance at the National Hospice and Palliative Care Organization (NHPCO), notes that the TEP recognized living situation and site of service as “important” risk adjustment recommendations.
“Identifying site of service will help to distinguish between care at home and care in a facility,” she says. Also vital, she continues, “is the recommendation from the TEP to consider length-of-stay as a risk-adjustment factor, including the differences between a 4-day length of stay and a 6-month length of stay.”
One TEP member cautioned that using payment sources, IV therapy, and risk of hospitalization as risk adjustors might tempt some hospices to use them to distort a hospices’ apparent care quality.
TEP members did not recommend using as risk adjustors gender, clinical symptoms, functional status and management of care needs. They did not discuss why they rejected gender, but several agreed that using clinical symptoms would not be of value because of their high correlation with diagnoses. Because hospice providers typically see hospice patients decline in ADL and IADL abilities, and hospice goals are focused on comfort rather than functional improvement, functional status was on the TEP’s “Do Not Include” as a risk adjustor list. And finally, one TEP member strongly opposed adjusting for patients’ medication management, supervision or safety assistance needs (management of care needs), explaining that “the public and CMS should hold hospices accountable for planning around oral medication, injectable medication management, and supervision and safety assistance,” the report says.
The TEP did suggest that using some risk adjustment factors as part of the HQRP could assist hospices internally with quality improvement while others would be more valuable to patients and families. For example, Patients and families would benefit from more straightforward risk adjustment that helps them select a hospice,” the report says, “including factors such as diagnosis. For publicly reported data used to select a hospice, the TEP suggested using demographic factors (including age but excluding gender), socioeconomic factors, living situation, and diagnoses.”
Dr. McNally hopes eventually to use HPRP data to promote Intermountain Hospice’s care. Intermountain Hospice is part of Intermountain Health, a health care provider with presence in multiple states. “You can’t take the current metrics to doctors’ offices and families to show anything meaningful,” he says. “It’d be great to have metrics we could take to our neurology docs and other docs,” he says. “I really think we provide better care and more options when patients stay within our system.
This article is the first in a series about implementation of HOPE. Next week, Beth Noyce shares details from the panel as it evaluated process measures.
# # #
©2024 by The Rowan Report, Peoria, AZ. All rights reserved. This article originally appeared in Healthcare at Home: The Rowan Report. One copy may be printed for personal use: further reproduction by permission only. editor@therowanreport.com

